“There is no comparison between DCISionRT and the Oncotype test for DCIS. As a radiation oncologist, to have a biosignature tool that gives me not only a risk without radiation, but risk with radiation, is invaluable and something that Oncotype doesn’t provide. So, it is a much more limited tool in my opinion. And the recognition that there is a difference in the magnitude of relative benefit to radiation across the biologic spectrum of DCIS is a very important piece of information that DCISionRT has uncovered.”
Troy Bremer, PhD, founder and CSO of PreludeDx, and Rachel Rabinovitch, MD, FASTRO, Professor of Radiation Oncology at University of Colorado, discuss DCISionRT and how it is used in the real-world clinical setting and the resulting changes in practice of precision medicine.
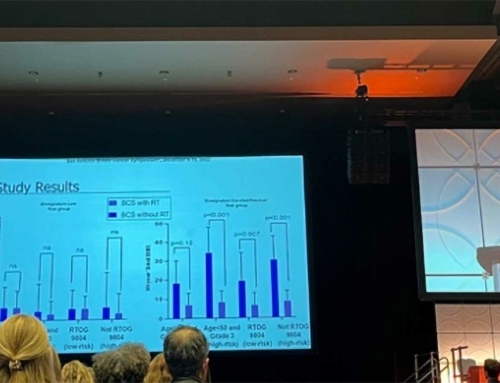
Dr. Rabinovitch started with background information on ductal carcinoma in situ (DCIS) also known as stage zero breast cancer and current treatment challenges. “There are nearly 50,000 new cases of DCIS annually and radiation is currently used as the default therapy following breast conserving surgery (BCS). We know that not every patient needs radiation, however it has been challenging identifying who does and doesn’t need radiation. Traditionally we have used very crude clinicopathological methods, such as grade, tumor size, margins and the age of the patient to decide. DCISionRT is the first precision medicine tool to help the physician and DCIS patient determine the need for radiation therapy following BCS in clinical practice.” Additionally, Dr. Rabinovitch reviewed landmark studies focused on DCIS in context of radiation therapy, including EBCTCG Overview, the ECOG 5194, RTOG-9804, and TROG/BIG DCIS studies.
Dr. Bremer shared an overview of the studies and clinical evidence to date for DCISionRT and radiation therapy. “First, DCISionRT was designed to fit into the normal process of treating a patient with DCIS and provide additional information. It integrates 7 biological markers with the traditional clinicopathologic factors. The test can be performed on a core biopsy or the surgical specimen after BCS. The test is for risk assessment of BCS alone and BCS with radiation. DCISionRT provides a Decision Score between 1 and 10. The score is translated into a set of risks. Importantly, we provide a second set of information, which is not available on any other test and that is risk following BCS and RT.”
“DCISionRT has been validated in approximately 1,500 patients and has been shown to be prognostic for 10-yr risk of recurrence, as well as predictive for radiation therapy benefit. In addition, as part of our ongoing PREDICT study (2,500 patients enrolled), DCISionRT changes the recommendation for radiation therapy about 40% of the time compared to clinical pathology.”
Dr. Rabinovitch next shared her experience as a radiation oncologist in the use of DCISionRT in clinical practice. “In my practice, I present my DCIS patients with prospective trial data and discuss the benefit of radiation based on their grade, margin status and age. I review if they are a candidate for partial breast radiation or not. But using the traditional data only gets me so far. So, my standard is to order DCISionRT for all of my patients to help us decide if radiation is needed or appropriate based on their individual tumor biology. The process is wonderfully smooth with results back in one week. Plus, the results are graphically very easy to see and understand.”
“I have been using the test for about 4 years and to date have ordered it on about 100 patients. I have a wide range of age, size and grade with 63% low risk and 37% elevated risk. Looking at the individual data, you can’t assume that age, size or grade can determine whether a patient has a low score or an elevated score. For example, results can vary widely over tumor size. You can have a very large tumor with a low risk of recurrence or a very small tumor with a very high risk of recurrence. So, the DCISionRT tool provides you with an individualized biosignature for each individual patient so you can more accurately understand where they fall on the continuum of biology.”
“Part of my patient cohort actually mirrors the 9804 low risk criteria. They are patients with grade I/II disease and lesion size of 2.5 cm or less. In this group, 38% of these traditionally classified low-risk patients were reclassified by DCISionRT to elevated risk, which predicts a much higher risk of recurrence without radiation and a substantial benefit with radiation. So DCISionRT really teases out these types of patients beyond what we can do just looking at a patient’s tumor grade or size. It is the only way to obtain quantifiable, predictive benefit of radiation therapy, beyond clinpath alone, to make an informed decision regarding radiation for myself and with the patient’s input. And I’m often surprised. With the 40% flip in treatment recommendations, my clinical judgement is pretty poor using traditional information. There is really no decision in medicine that you would want to rely on if you knew that you were going to be wrong that often. So, I think that it is just a fantastic test.”
“Oncotype is a test that most people know of, but I think that there is no comparison between DCISionRT and the Oncotype test for DCIS. As a radiation oncologist, to have a biosignature tool that gives me not only a risk without radiation, but gives me a risk with radiation, is invaluable and something that Oncotype doesn’t provide. Oncotype only gives you a risk without radiation because their data was based on the ECOG 5194 study, which didn’t use radiation. So, it is a much more limited tool in my opinion. And the recognition that there is a difference in the magnitude of relevant benefit to radiation across the biologic spectrum of DCIS is a very important piece of information that DCISionRT has uncovered.”
“I want to make this point to my fellow radiation oncologists. DCISionRT is at a very similar point as Oncotype when it was widely adopted for chemotherapy for life-threatening occult metastatic disease. DCISionRT has been tested on multiple cohorts, as well as a randomized trial. To me the data is very consistent and very clean and something that is ready for use in your clinic for any of your DCIS patients.”
Dr. Rabinovitch provided some advice on how to get started with the test. “I consider DCISionRT a test within the radiation oncologist’s domain, however I know a number of breast surgeons who order it. In fact, as part of our tumor board, my surgeons let me know when a DCIS patient is coming along so I can get it ordered. I work with our pathologist who submits the sample. I simply fill out a very simple 1-page editable PDF form. My assistant sends in the pathology and the insurance information.”
Dr. Rabinovitch concluded her presentation with several case studies, with similar clinpath (age, size, grade) but different DCISionRT outcomes, that highlighted how often she is surprised by the DCISionRT results.
To listen to the entire webinar, click https://bit.ly/3Aeetzn
Troy Bremer, PhD – PreludeDx Founder and Chief Scientific Officer
Rachel Rabinovitch, MD, FASTRO – Professor, Radiation Oncology, University of Colorado