“Once I started incorporating DCISionRT®, I was able to more accurately identify patients who would benefit from radiation therapy and those who could safely omit radiation therapy.”
Troy Bremer, PhD, Chief Scientific Officer, PreludeDx; James Pellicane, MD, Director of Breast Oncology, Bon Secours Cancer Institute; and David Rock, MD, Breast Surgeon, GenesisCare, discuss the latest SweDCIS randomized data and how they are implementing DCISionRT in their practices.
Dr. Bremer kicked off the meeting with a discussion of the current challenge of overtreatment with radiation therapy for ductal carcinoma in situ (DCIS). “Specifically, about 80% of DCIS patients treated with breast conserving surgery (BCS), and no other adjuvant therapy, don’t recur. Yet, 80% – 90% of DCIS patients are treated with other adjuvant therapy, including radiation therapy (RT), following BCS due to a lack of confidence in who actually needs adjuvant therapy. This overtreatment substantially impacts quality of life for women with DCIS and results in a high cost of radiation to the health system.”
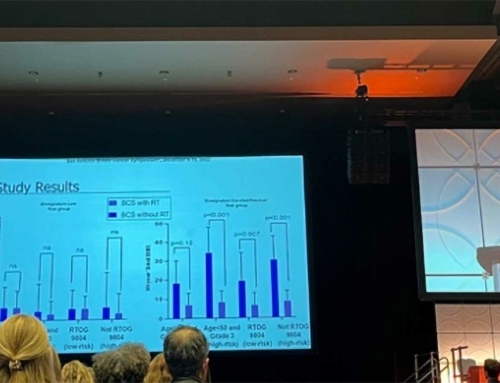
“When we look at the data in aggregate across three studies, and 1,500 patients, the question is ‘how much benefit from RT are you getting in the low-risk group’? When we look at a ten-year risk profile for an invasive risk reduction with RT, it is only a 1 – 2% RT benefit for the DCISionRT low-risk group.”
This current scenario could be avoided with a better tool to assess DCIS risk and radiation benefit, resulting in a personalized treatment. The DCISionRT test takes a series of different biomarkers, along with clinicopathology to provide a comprehensive result for risk that clinicians and patients can use to make a decision.
Dr Bremer continues, “It’s important to point out that traditional clinicopathology does not give you enough information to confidently classify a patient as low risk or elevated risk. For example, in multiple studies, 40 – 50% of ‘good-risk’ clinpath were reclassified by DCISionRT to elevated risk. Whereas 30 – 40 % of ‘high-risk’ clinpath were reclassified by DCISionRT to low risk.”
What does this mean in terms of implementation?
Dr. Rock shared his experience from when he moved to Florida. “I was using clinpath to determine who I should send to radiation, which as I have learned from participating in the PREDICT study was basically a coin toss.”
“Once I started incorporating DCISionRT, I was able to more accurately identify patients who would benefit from radiation therapy and those who could safely omit radiation. From a breast surgeon perspective, it is valuable to have the DCISionRT results before surgery if the patient is in an elevated-risk group with residual risk following radiation. That patient may opt for a mastectomy versus breast conserving surgery.”
“So, the key is that you must run DCISionRT on everybody. You will spare patients from RT who may not derive a significant benefit. Similarly, DCISionRT will help us better identify which patients are at the highest risk and will have significant benefit from RT.”
Dr. Pellicane discussed several cases where the patient had a predetermined mind set that resulted in a changed treatment decision following DCISionRT. “In my practice, I never want to talk a patient out of their decision, but I want them to have all the information before surgery. So, this is another way to use DCISionRT pre-operatively.”
DCISionRT testing can be performed on the pre-surgical/core biopsy or the lumpectomy specimen.
“My lessons learned after using DCISionRT is that the test provides you additional information beyond estrogen receptor status or grade that will impact treatment decisions. In terms of adoption, it takes a while to garner buy-in from all members of the care team and with the latest SweDCIS randomized data, PreludeDx is at that point of having collective buy-in. And importantly, treatment should be personalized and based on biology, not just solely on Clinpath.”
“I order DCISionRT on everybody because I am trying to get a risk assessment, as well as a therapeutic benefit assessment. And as I previously shared, more information makes for better consultations. DCISionRT on core biopsy can clarify risk and lead to more informed shared surgical decision making. It can also guide post-op hormonal therapy given invasive risk.”
Biggest roadblocks for surgeons
Dr. Pellicane concluded, “DCIS is essentially a surgical disease and a risk marker for developing invasive ductal carcinomas, so we need to change old habits. We also must eliminate clinical bias versus biology and ‘selective ordering’. Younger, intuitively ‘high-risk’ patients may not need radiation. And older, healthy patients may be at significant risk of invasive recurrence. So, my advice is to stop the selective ordering and order it on all reasonable DCIS patients.”
For additional clinical information on DCISionRT and how it is being implemented in practices, click here to watch the video presentation: https://youtu.be/5rHjf7khJzc