“In our practice we are still radiating the same number of patients, but with DCISionRT we are treating the right patients.”
Leonard A. Farber, MD, Radiation Oncologist and Beth DuPree, MD, FACS, ABOIM, Breast Surgeon join Dede Goehler, BSN, PreludeDx Patient Advocate to discuss how physicians can leverage the latest precision medicine technology to determine which ductal carcinoma in situ (DCIS) patients will benefit from radiation therapy (RT) following breast conserving surgery (BCS) and which patients can safely omit RT. In addition, the physicians share real-world patient case studies of how DCISionRT helps determine a personalized treatment plan.
Current standard of care for DCIS begins with an abnormal mammogram followed by a biopsy. The patient receives their diagnosis of DCIS and based on the breast conservation approach, the patient undergoes breast conserving surgery. And then the big question is ‘is the patient referred for radiation therapy? And if so, who really needs radiation therapy?’
Again, under the standard treatment of DCIS, clinicians have historically used clinicopathology factors, such as age, size of tumor, grade, and margin status to determine low risk factors. Under the most recent National Comprehensive Cancer Network (NCCN) guidelines, if the patient and physician view the individual risk as ‘low,’ some patients may be treated by excision alone. But how do physicians detect low risk?
Where does DCISionRT fit into clinical decision making?
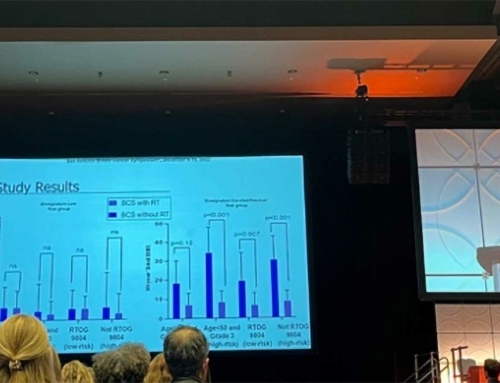
Dr. Farber explains, “DCISionRT comes into play after breast conservation surgery, and also plays a role after biopsy, before deciding treatment strategy, for lumpectomy and intra-operative radiation therapy. It is an assessment tool to personalize treatment. Patients are given a score. A Decision Score (DS) of 0 – 3 is deemed low risk and has been demonstrated to have low to minimal benefit with RT. A DS of greater than 3 to 10 yields a high relative RT benefit.”
“DCISionRT has a high clinical impact with extensive validation, which is critical for physicians,” says Dr. Farber. “As well, the DS is a concrete score that physicians can share with their patients to guide RT treatment decisions. And clinical utility studies demonstrate the decision impact of DCISionRT on physicians’ treatment recommendation, resulting in an overall change in adjuvant RT recommendations over 40% of the time.”
The surgical perspective
Dr. DuPree continued the presentation by sharing her desire as a breast surgeon to find the very best path forward for every patient – meaning she doesn’t want to overtreat or undertreat patients. “Often times patients are plugged into categories based on age or grade or size of tumor. DCISionRT has been very helpful for me in surgical planning. For example, I have some young patients who really do not want to get RT, but a high DS may be a reason for them to proceed with a mastectomy versus a lumpectomy.”
In Dr. DuPree’s practice, breast care is a multi-disciplinary collaboration between the entire cancer care team. She especially highlighted the nurse navigator role as the “glue” between the various specialties and the patient’s advocate on their cancer journey. In addition to playing a key role in her treatment recommendations for DCIS, Dr. DuPree emphasized, “DCISionRT gives the radiation oncologist a tool to have an educated discussion with the patient. In our practice we are still radiating the same number of patients with RT, but with DCISionRT we are treating the right patients. And DCISionRT gives our patients the confidence to move forward with the appropriate treatment.”
“As physicians we need to ‘do no harm’, but we also need to use the high-tech technology available to us to make better treatment decisions,” concluded Dr. DuPree.
For additional clinical information on DCISionRT, how it is differentiated from OncotypeDx DCIS, and how surgeons and radiation oncologists are implementing it into their practices, click here to watch the webinar https://preludedx.com/webinar/.