So, you or a loved one has been diagnosed with breast cancer… now what?
First and foremost, we are so terribly sorry you ever had to hear those words. Whether the diagnosis is yours or it’s a parent, child, friend or family member’s, it’s a scary time for everyone involved.
Education is arguably the most important tool with which to arm yourself when facing a breast cancer diagnosis, but the learning curve can be overwhelming at first. So to start, let’s break down one of the fundamentals of a breast cancer diagnosis and a large percentage of what goes into staging, treatment recommendations and overall risk: is the tumor invasive or non-invasive?
First, a quick anatomy refresher. Within each breast, there are usually between 15 and 20 lobes comprised of many smaller glands called lobules, and it’s these lobules that produce milk in nursing women. To get the milk from the lobules to the nipple, there is somewhat of a pipe system made up of small tubes called milk ducts that connect to the areola. Surrounding this conveyor belt system, just on the other side of the lobules and ducts, is presumably healthy tissue that varies in density depending on the woman.
When cells go haywire and become tumors, they most often start in either a duct or lobule as opposed to developing directly amid the breast tissue. The specific type of breast cancer that is diagnosed relies on two things: where the tumor originated and whether or not it is still contained there.
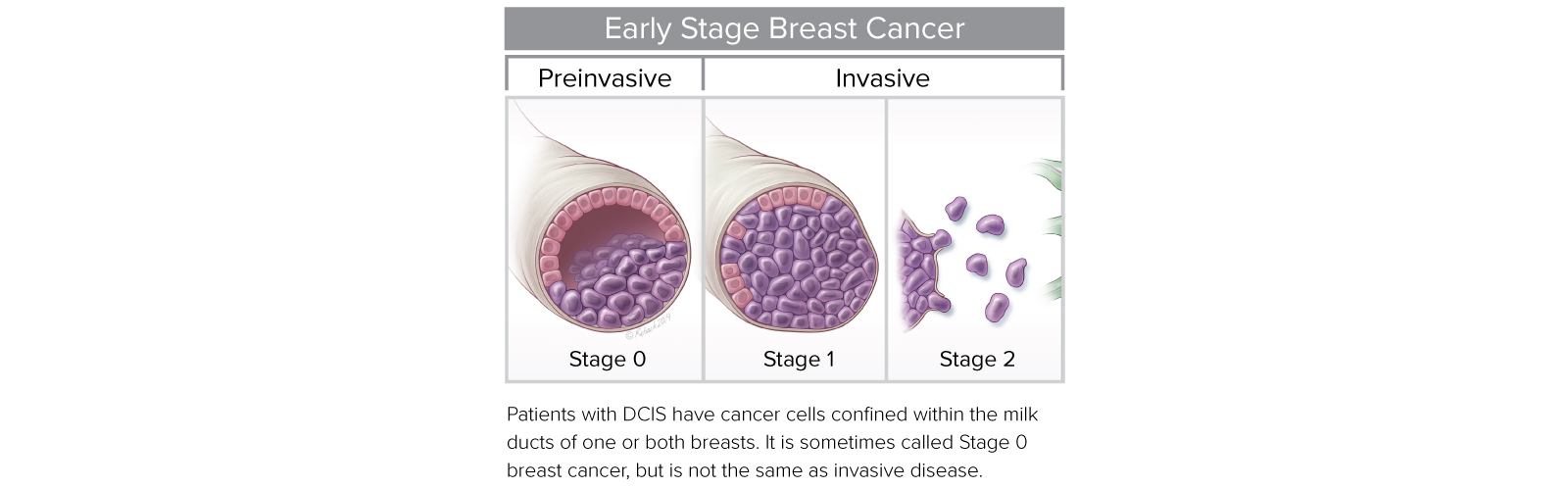
A tumor that originates in one of the patient’s milk ducts will be referred to as “ductal” and a tumor that originates in a lobule will be called “lobular”. If either of those tumors have not yet “broken through” the walls of the duct or lobule and begun to grow into the tissue on the other side, the cancer is considered “non-invasive” and your doctor will tack on the words “in situ”– the latin phrase for “on site” or still “in position”– to the end of your diagnosis, creating the more well-known acronyms of DCIS (ductal carcinoma in situ) and LCIS (lobular carcinoma in situ). All non-invasive breast cancers are considered to be stage 0. On the other hand, if the tumor has broken through the walls of the duct or lobule, it is now considered to be “invasive” and will now fall somewhere between stage 1 and stage 4 based on a number of different factors.
However, it’s important to understand that a non-invasive, stage 0 diagnosis is not indicative of how aggressive a tumor is, but rather just how early it was caught. Just as breast size varies from woman to woman, so do lobule size and duct size. Five mm of tumor on one woman might still be non-invasive and the same size on another woman might be invasive. Tumors can be 25 mm in size, but fairly tame on a genomic level, meaning if you remove them, they likely won’t come back. Others might be only 2 mm and barely detectable, but more aggressive, and potentially require more treatment.
The one and only way to know which is which, is to have your doctor order genomic testing such as DCISionRT to be done on the tumor. Click here for more information on genomic testing and why it is so crucial when approaching treatment decisions for DCIS.