Dr. Farber has had a decorated career having held faculty and physician positions at some of the leading research institutions including Memorial Sloan Kettering Cancer Center, City of Hope/St. Jude Cancer Center, and the Weill Cornell Medicine. Today he serves as the Chief Medical Officer of EHMET Health and Senior Medical Director and Section Chief of Radiation Oncology at Care to Care, LLC.
“As a practicing radiation oncologist, conversations with my ductal carcinoma in situ (DCIS) patients pre-DCISionRT® were always, ‘you are in a grey zone’. I just didn’t have a test that would give me a definite answer as to which patient would benefit from radiation therapy.”
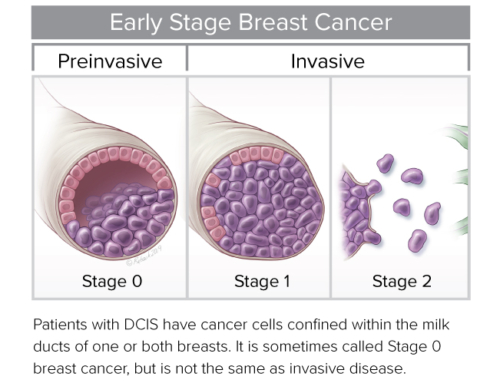
DCISionRT, developed by PreludeDx™, is the only risk assessment test for patients with DCIS that predicts radiation therapy benefit. The test provides a Decision Score that identifies a woman’s risk as lower or more elevated.
“Personally, I have always been interested in being on the forefront of technology if it benefits patients. For me, DCISionRT was the first time there was real data to make decisions regarding radiation therapy. From the point I learned of DCISionRT, I started to prescribe the test for every DCIS patient.”
Dr. Farber joined PreludeDx as a Senior Clinical Advisor in 2019. In this role, he consults with physicians and patients regarding the implementation of DCISionRT in the treatment planning for DCIS patients.
“I knew DCISionRT was going to be a paradigm-changer for radiation oncology, and I really needed to be a part of it. I also knew that it was going to be a slow process to change physicians’ minds and how they utilize radiation therapy in the treatment of DCIS. We had to convince them. And the most important step was to validate the new technology with data. This is why the recent randomized SweDCIS study data is so important for the acceptance and widespread adoption of DCISionRT.”
Radiation has been an effective tool for treating cancer for more than 100 years. More than 60 percent of patients diagnosed with cancer will receive radiation therapy as part of their treatment. That number goes to 70 – 80 percent for breast cancer patients.
Radiation therapy is the delivery of external beam radiation treatments. It works by damaging the DNA of cells and destroying their ability to reproduce. Both normal and cancer cells can be affected by radiation, but cancer cells have generally impaired ability to repair this damage, leading to cell death. All tissues have a tolerance level, or maximum dose, beyond which irreparable damage may occur. When radiation oncologists administer radiation therapy, they strive to provide the appropriate dose that kills cancer cells while causing the most minimal damage to healthy tissue as possible.
Many patients today receive fractionation therapy. This is where radiation oncologists divide the total dose into small daily fractions over days to weeks. Fractionation takes advantage of differential repair mechanisms of the normal and malignant tissues. It also spares normal tissue through repair and repopulation while increasing damage to tumor cells through redistribution and reoxygenation. “This is a growing trend. We are moving to the direction of increased use hypofractionation because we have found comparable or superior response in many clinical scenarios.”
Radiation therapy plays a major role in the management of many common cancers either alone or as a neoadjuvant/adjuvant therapy with surgery, chemotherapy, and immunotherapy.
“The patient is referred to the radiation oncologist from the breast surgeon, medical oncologist, radiologist, or direct referral for a consultation, which we are seeing more of lately. If they opt for radiation, next they go for a simulation. The simulation is really the first part of the treatment process where the patient undergoes a CT or MRI scan in the treatment position and reference marks or ‘tattoos’ may be placed on the patient and images are forwarded for treatment planning.”
The effects of radiation therapy are cumulative with most significant side effects occurring near the end of the treatment course and unlike the systemic side effects from chemotherapy, radiation therapy is limited to the site of treatment. Common side effects for breast radiation may include swelling, skin redness, and cosmetic alterations.
“Today, thanks to DCISionRT, not all patients will automatically progress to radiation therapy. DCISionRT allows us to differentiate who the patients are that will benefit most from radiation therapy. This enables some patients to safely forego radiation and avoid the side effects and retain the treatment option of radiation therapy down the road if it becomes necessary.”