“In this webinar, Eric Brown, MD, FACS; Erica Giblin, MD; James V. Pellicane, MD; Troy Bremer, PhD; and Leona Hamrick, DHSc, PA-C, MSL-BC, discuss how DCISionRT and its newly integrated Residual Risk Subtype (RRt) played a significant role in treatment decision making in DCIS patients identified in the RRt category. These key opinion leaders discuss actual patient cases with RRt, the differentiating factors among cases, patient preference and final treatment decisions.”
Background and DCISionRT Overview
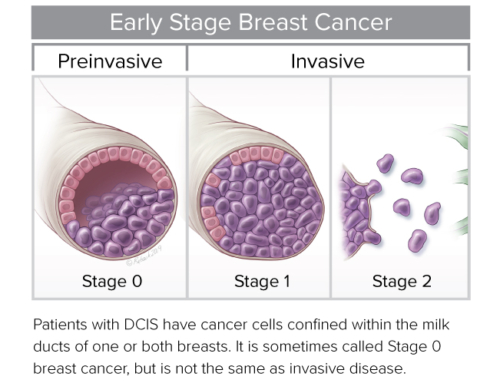
PreludeDx brings together key opinion leader surgeons to address three of the key questions for ductal carcinoma in situ (DCIS) management. Who are the patients who have elevated recurrence risk after breast conserving surgery (BCS)? Who are the patients who will and will not benefit from radiation therapy (RT)? Who are the patients at higher risk after BCS plus RT?
Troy Bremer, PhD, Founder and Chief Scientific Officer, PreludeDx, reviewed published data from four randomized clinical trials that demonstrate that the DCISionRT test is predictive and prognostic for RT benefit with multiple confirmations. Dr. Bremer stressed that the test objective is to provide additional information beyond what you would normally have with clinical pathology to be able to make an assessment about patient risk and the benefit from RT for DCIS. “The DCISionRT test, performed on the core biopsy or surgical specimen, can aid in personalized treatment decisions.”
Leona Hamrick, DHSc, PA-C, MSL-BC, Senior Director of Global Medical Affairs, PreludeDx, provided an interesting comparison of the validation cohort patient distribution and real-world global clinical testing patient distribution from the last 18 months. “What I want to draw your attention to is the concordance in those low, elevated and Residual Risk groups. So, for clinical practice that means that DCIS patients shouldn’t be treated the same just because they have a DCIS diagnosis. For example, as highlighted in the Red Journal article, that Residual Risk subtype with an elevated recurrence risk remaining after BCS plus RT, could warrant potentially intensified or alternative treatment approaches, such as different surgical considerations, including wider margins or mastectomy; increased use of boost or modified boost dose.”
Patient Case Studies
James Pellicane, MD, Director of Breast Oncology Bon Secours Cancer Institute, kicked off the patient case studies review. “Our practice covers a wide area in Central Virginia and I’m excited to share a few key case studies. I will be sharing my opinion on ‘why we order DCISionRT? When we order it on the surgical specimen and how does it change our treatment and how do we utilize that in our practice?’
“One of the important things for me is that we treat invasive breast cancer based on biology, so DCISionRT is a natural progression on how we treat DCIS based on biology vs. clinical factors alone. An eye opener for me is that we used to think that DCIS is an early breast cancer, when in fact, it is a different disease from early-stage invasive breast cancer. We don’t know which DCIS cases will progress to invasive breast and although there are ongoing trials trying to answer this question, until we have some results, we need to treat them all as if they will progress, especially in younger patients. This test does not necessarily give us an idea of who will progress from DCIS to invasive upon diagnosis, but it gives us the ability to determine which DCIS cases may recur after breast conserving surgery. It has turned the old school thinking of ‘50% will recur, drop it by 50% with radiation and 50% will come back as invasive’ on its head. So, knowing that DCIS is a different disease, this test has enabled us to make some good decisions and advocate on behalf of our patients as it relates to offering radiation therapy and in some cases mastectomy. In fact, we order DCISionRT for every DCIS patient because knowing each patient’s individual risk helps us to make better recommendations for our patients.”
Dr. Pellicane presented 4 cases with Residual Risk subtype that approached their DCIS diagnosis from different perspectives. “My first case study is a 61-year-old female who came to see me when she was unable to have a stereotactic biopsy because she was very thin with small breasts and breast implants. We took her to the operating room for an excisional breast biopsy. Her biopsy revealed DCIS, intermediate grade with a 7mm size and clear margins and was ER+/PR+. We ran DCISionRT on her surgical specimen and it came back with a Residual Risk type. She had already had her surgery and she had clear margins, so her decision tree was either radiation therapy or mastectomy. She had zero risk tolerance with respect of recurrence. After a lot of discussion, she decided to undergo bilateral mastectomies with immediate reconstruction. The important point here is that we focus on all recurrence, but we really focus on invasive recurrence because that is what is important to a lot of patients and physicians. Even though 7 percent invasive recurrence risk after radiation therapy sounds low to some patients, for other patients it is just too high.”
Next, Erica Giblin, MD, Medical Director Breast Care Services, Breast Surgical Oncologist at Ascension Medical Group in Indianapolis, shared her perspective. “We see about 500 breast cancers/year. I order DCISionRT on all my DCIS patients; I do not cherry pick. I am a big fan of ordering DCISionRT on core biopsy specimens and I will share how I feel the test can help as I go through these cases.”
“I had a 42-year-old female physician/patient that underwent a screening mammogram that showed extremely dense breast tissue and a cluster of calcifications in the left breast. She underwent a stereotactic core biopsy that revealed hybrid DCIS ER+/PR+. I ran DCISionRT on her core biopsy specimen, which came back high residual risk. In her case, I ran the test on the core biopsy specimen because when I initially consulted with her she was adamantly against radiation therapy. So, by running the test on the core biopsy specimen it was an asset to determine if she would require radiation therapy or not if she were to pursue breast conservation surgery. Due to the high residual risk, she decided to get a nipple sparing mastectomy. So, for this physician/patient DCISionRT was instrumental in decision making for her surgery given her personal preference to avoid radiation therapy at all costs.”
“I have a significant number of DCIS patients that are initially very resistant to the idea of radiation therapy. So, having a discussion with them where I can show them numerical data in terms of risk of recurrence with and without radiation therapy – that blows their minds. And they grab on to that and that helps the decision-making process go so much easier for the surgeon, the patient and the radiation oncologist. It is a huge asset.”
Eric Brown, MD, FACS, Leader, Breast Cancer Multidisciplinary Team, Comprehensive Breast Care, a Division of Michigan Healthcare Professionals, closed out the case study discussion with 4 patient studies. “We are a 500-doctor private practice group, and we treat about 1,100 breast cancers a year.”
“My patient is a 68-year-old female that presented with a screen detected calcification in her left breast that spanned about 2.5 cm. She had a stereotactic core biopsy that revealed a Grade II DCIS. She had no preference with regards to radiation therapy but was interested in breast conservation. We did a lumpectomy where we found an additional 3 mm of intermediate grade DCIS. She had clear margins. Pre-DCISionRT, the recommended treatment was lumpectomy. When we looked at her DCISionRT report and saw that she had Residual Risk, we altered our treatment plan to lumpectomy plus radiation plus boost. Our radiation oncologists tend to prefer a boost for DCIS Residual Risk patients who choose a lumpectomy and radiation therapy.”
“We also order the DCISionRT test for all our DCIS patients. Our radiation oncologists are on board and recognize that it is bad economically when you radiate every patient, especially for large practice groups. And patients love the test. The report is very easy to read and easy for the patients to understand. So, it has been a huge asset for us.”
To listen to the entire webinar, including a comprehensive overview of clinical data and case studies and questions, click Webinar
James Pellicane, MD, Director of Breast Oncology Bon Secours Cancer Institute
Erica Giblin, MD, Medical Director Breast Care Services, Breast Surgical Oncologist at Ascension Medical Group in Indianapolis
Eric Brown, MD, FACS, Leader, Breast Cancer Multidisciplinary Team, Comprehensive Breast Care, a Division of Michigan Healthcare Professionals
Troy Bremer, PhD, Founder and Chief Scientific Officer, PreludeDx
Leona Hamrick, DHSc, PA-C, MSL-BC, Senior Director of Global Medical Affairs, PreludeDx