“In this webinar, Chirag Shah, MD; Fleure Gallant, MD; Lonika Majithia, MD; Leona Hamrick, DHSc, PA-C, MSL-BC; and Troy Bremer, PhD, discuss how DCISionRT and its newly integrated Residual Risk Subtype (RRt) played a significant role in treatment decision making in DCIS patients identified in the RRt category. These key opinion leaders discuss actual patient cases with RRt, the differentiating factors among cases, patient preference and final treatment decisions.”
Background and DCIS Clinical Need
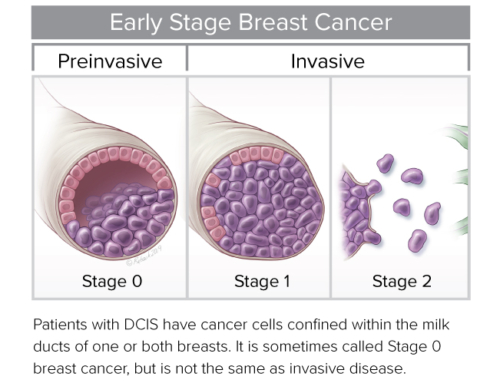
Key opinion leaders gathered to participate in a round table discussion on DCISionRT® and its role in identifying ductal carcinoma in situ (DCIS) patients who will and will not benefit from radiation therapy (RT) following breast conserving surgery (BCS), and the primary focus of this webinar, DCIS patients who remain at high risk of recurrence after BCS and RT.
Leona Hamrick, DHSc, PA-C, MSL-BC, Senior Director of Global Medical Affairs, PreludeDx, kicked off the webinar with a historical perspective of DCIS Landmark Trials that demonstrated radiation therapy reduced the rate of ipsilateral breast events (IBR) by about 50% following BCS. However, 72% of patients had no recurrence without RT, leaving the question ‘how do we determine which patients will benefit from radiation therapy’? Next Dr. Hamrick introduced DCISionRT, a molecular test performed on core biopsy or surgical specimen, designed to provide additional information, including 10-year total risk of recurrence (DCIS and invasive combined) and 10-year risk of recurrence of invasive alone for BCS and BCS+RT, to aid the clinician and patient in more personalized, shared decision-making.
According to Dr. Hamrick, “the DCISionRT biosignature test combines 7 biomarkers and 4 traditional clinicopathologic factors – age, palpable, lesion extent and margin status – to achieve a significantly validated, prognostic risk of an in-breast recurrence and predictive benefit of radiation therapy.”
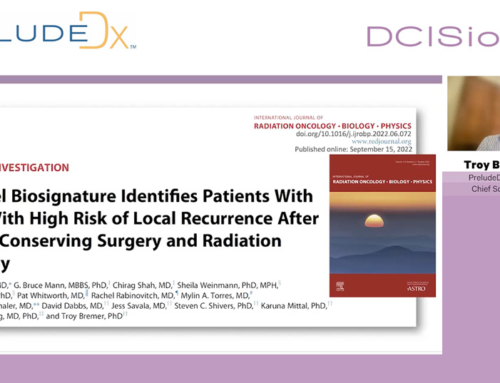
Next, Troy Bremer, PhD, Founder and Chief Scientific Officer, PreludeDx, reviewed published validation studies that demonstrate that the DCISionRT test is predictive and prognostic with multiple confirmations. Dr. Bremer highlighted the most recent data from the Red Journal that evaluated patient distribution by DCIS Biosignature Risk groups, including a low-risk group, elevated risk group, and a residual risk group – those patients who remain at a high risk following BCS and RT. “What we have found in our studies is that DCISionRT reclassifies 44% – 51% of patients who are ‘low-risk’ clinicopathology (RTOG 9804-like) into the elevated risk group and 7% of clinicopathology ‘low-risk’ patients into the residual risk group. So, what we are showing is that even within the ‘low-risk’ clinicopathology, many patients do have a high risk that can be identified by molecular biology. Conversely, when we look at patients who do not meet the RTOG 9804 criteria, we see that 23% of those patients are reclassified into the low-risk group using DCISionRT and 34% of patients are reclassified into the residual risk group.”
Dr. Bremer concluded his talk by reviewing DCISionRT’s supportive evidence demonstrating that the test is prognostic for 10-year risk of recurrence, predictive for RT benefit and highly consistent across all studies. “Within 1,600 patients and 5 cohorts, DCISionRT has demonstrated stratification for risk and RT benefit. The DCISionRT ‘true low risk group’ has no significant RT benefit, the ‘elevated group’ has targeted RT benefit and risk reduction, and the ‘residual risk group’ has significant risk despite substantial RT benefit.”
Patient Case Studies
Chirag Shah, MD, Co-director of Comprehensive Breast Program and Director of Clinical Research in the Department of Radiation Oncology at Cleveland Clinic, was the first clinician to discuss why he orders DCISionRT, how it impacts patient perspectives and clinician perspective regarding shared decision making, and how he implemented it into his practice. “I was a co-author on the Red Journal publication addressing residual risk patients with an elevated recurrence risk remaining after breast conserving surgery plus RT and potentially warranting intensified or alternative treatment approaches. Authors of the paper discuss residual risk patients may be considered for tumor bed boost, additional systemic therapies, and/or clinical trials, as well as different surgical approaches, increased use of boost or modified boost dose, and HER2 targeted therapies (for HER2[3+] patients).”
Dr. Shah highlighted a case study of a 63-year-old female with high grade DCIS measuring 10 mm. “The patient had negative margins, non-palpable and was ER+. She was adamant about not having radiation even though that was the recommendation given all her factors. We ordered the DCISionRT test, which came back high risk (RRt) and she decided to have a mastectomy. So, in this case, DCISionRT influenced her surgical management.”
Next, Fleure Gallant, MD, Clinical Director of Radiation Oncology, Maimonides Medical Center, Clinical Assistant Professor, SUNY Downstate Medical Center, discussed a residual risk subtype case focused on an older patient. “The patient, age 78, came in with a preconceived notion of ‘no radiation’ after breast conservation based on a diagnosis of stage zero breast cancer. She was ER-/PR- so I was hopeful that she would be in the category that could safely omit radiation. However, when we received her DCISionRT score, she was in the high-risk (RRt) group with a 40% risk of recurrence without radiation. So, with the DCISionRT score, I was able to convince her to get radiation and we moved forward with an ultra-hypo fractioned regimen with a boost. So, this was definitely a case where seeing those high risk of recurrence numbers changed a patient’s thinking and treatment decision.”
Lonika Majithia, MD, Medical Director of Brachytherapy & Director of Radiation Oncology Educational Program at Inova Schar Cancer Institute closed out the case study discussion with 4 patient studies. “This patient case study is a 53-year-old female with a high grade, 6 mm lesion. She was ER+ with negative margins. She had a family with young children and wanted to be as aggressive as possible with treatment. She originally wanted a mastectomy but was convinced to do a lumpectomy by her breast surgery team and she wanted to do radiation. In this case, DCISionRT added another layer of information to help her make her decisions which included whole breast radiation without a boost, oncoplastic reconstruction and tamoxifen.”
The webinar concluded with a dynamic roundtable discussion and sharing of opinions among all panel members regarding their patient case studies.
To listen to the entire webinar, including case studies and questions, click here
Chirag Shah, MD, Co-director of Comprehensive Breast Program and Director of Clinical Research in the Department of Radiation Oncology at Cleveland Clinic
Fleure Gallant, MD, Clinical Director of Radiation Oncology, Maimonides Medical Center, Clinical Assistant Professor, SUNY Downstate Medical Center
Lonika Majithia, MD, Medical Director of Brachytherapy & Director of Radiation Oncology Educational Program at Inova Schar Cancer Institute
Troy Bremer, PhD, Founder and Chief Scientific Officer, PreludeDx
Leona Hamrick, DHSc, PA-C, MSL-BC, Senior Director of Global Medical Affairs, PreludeDx