“In this webinar, Dr. Pat Whitworth, MD, FACS, Chirag Shah, MD, and Troy Bremer, PhD, provide an overview of recently published data in the Red Journal of PreludeDx’s DCISionRT and its newly integrated Residual Risk Subtype (RRt). These key opinion leaders discuss DCISionRT and its role in identifying truly low-risk ductal carcinoma in situ patients who receive no benefit from radiation therapy (RT) following breast conserving surgery (BCS), as well as DCIS patients who remain at elevated risk of recurrence after BCS and RT.”
Background and DCIS Clinical Need
Pat Whitworth, MD, FACS, Breast Surgical Oncology Specialist and Director of the Nashville Breast Center; Chirag Shah, MD, Co-Director of Comprehensive Breast Program and Director of Clinical Research in the Department of Radiation Oncology at the Cleveland Clinic; and Troy Bremer, PhD, Founder and Chief Scientific Officer, PreludeDx, discuss DCISionRT® and its role in identifying truly low-risk ductal carcinoma in situ (DCIS) patients who receive no benefit from radiation therapy (RT) following breast conserving surgery (BCS), as well as DCIS patients who remain at elevated risk of recurrence after BCS and RT.
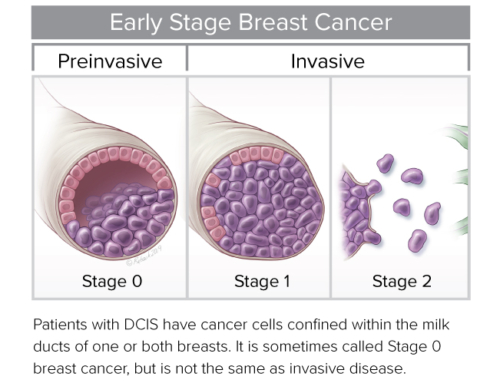
Dr. Whitworth kicked off the webinar with a historical perspective of DCIS Landmark Trials (NSABP, EORTC, UK/ANZ, and SweDCIS) that demonstrated radiation therapy reduced the rate of ipsilateral breast event rates (IBR) by about 50% following breast conserving surgery (BCS). And 30% of patients have a recurrence without radiation (half were DCIS and half were invasive). Dr. Whitworth recognized that radiation therapy impacts the quality of life for the patient and patients prefer to not have radiation if it is of no benefit to them.
According to Dr. Whitworth, “the question we must answer is ‘how do we identify the 70% of patients who don’t recur in 10 years with BCS alone’? We really want to identify these folks, because if we can do that well, they don’t need radiation and the worry and complications that come with it. In fact, 85% of patients did not have an invasive breast cancer recurrence after BCS alone. However, a substantial majority of patients are treated with BCS plus RT.”
“For many, many years, we have used grade and age as the primary criteria to identify patients who have such a low risk that they don’t need RT. And a number of other efforts have been made to identify truly low-risk patients. But until we had genomic analysis to reveal the biology of the lesion, we really didn’t have an accurate tool to identify those patients, until now.”
About DCISionRT
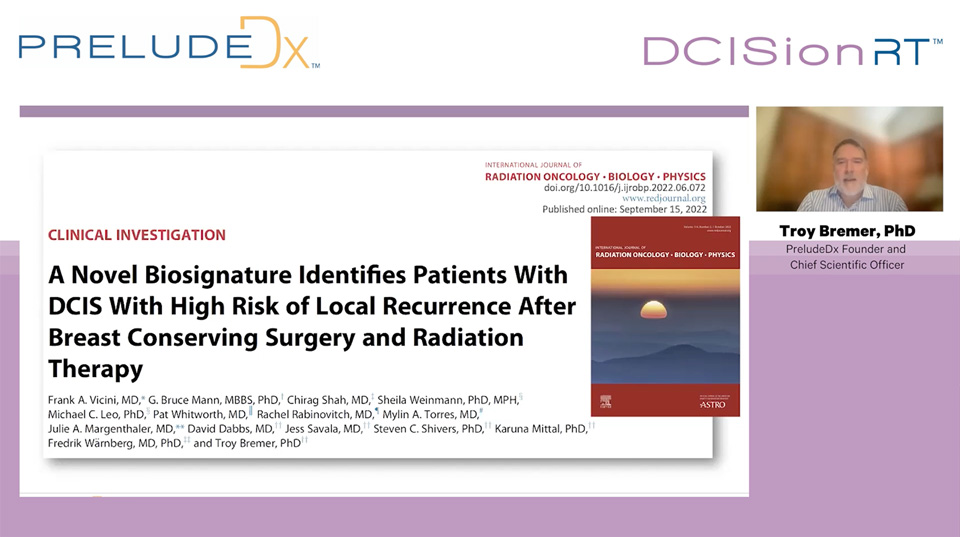
Next, Dr. Bremer introduced DCISionRT, a 7-gene predictive DCIS assay for RT. “The Decision Score (DS) is the result of an algorithm that combines 7 biomarkers with 4 clinicopathologic factors. DCISionRT is validated as prognostic for IBR risk and predictive for RT benefit in Level 1b evidence. The test can be performed on a core biopsy or the surgical specimen after BCS. The test is for risk assessment of BCS alone and BCS with radiation. DCISionRT provides a Decision Score between 1 and 10. The score is translated into a set of risks. Patients with an elevated DS have 70% relative risk reduction with RT and patients with a low DS have no significant RT benefit.”
Dr. Bremer introduced an additional question for the test to address – which patients have significant residual risk despite BCS plus RT? “When we examined the biomarkers for this group of patients, we observed that most of these patients were Her2Neu positive. Our hypothesis was an activated K-RAS pathway may identify patients with high residual risk after BCS and RT. So, we developed a second algorithm that pre-specified the hypothesis and combined the set of DS biomarkers into a novel Residual Risk Subtype (RRt). So, with DCISionRT, we now have an algorithm that gives you a continuous risk score, as well as an additional interactive (non-linear) algorithm integrating K-RAS pathway biomarkers that provides a residual risk subtype.”
DCISionRT Clinical Evidence
Dr. Chirag Shah, MD then discussed how DCISionRT and the RRt was validated. “The study population was a pooled multinational cohort of 926 patients with 10-year follow-up. Patients were divided into three risk groups via the DCISionRT test – Low risk (37%), Elevated Risk (43%), and Residual Risk (20%). So, it is one thing to understand a patient’s risk, it is a different question to understand a patient’s benefit from RT. When we examined the three cohorts, DCISionRT was shown to be prognostic for IBR rate and prognostic and predictive for RT benefit. In the low-risk group, we saw no significant RT benefit. In the elevated-risk group, we saw a clear benefit to RT. In the residual risk group, we saw a 27% benefit in recurrence, but also a relatively high risk of recurrence.”
“This information translates clinically to answer the question of ‘how many patients do I need to treat with RT to help 1 patient. In the low-risk group, if you radiated 100 patients, you would only help 1 patient. That is 1% and clearly no value. That number goes to 6 patients to help 1 in the elevated risk group and 4 patients to help 1 in the RRt group.”
“I think that it is also important to point out that the RRt is not all high-risk patients, but low risk clinicopathology features are actually showing up in RRt patients. That seems illogical, but that is why the test is discriminating something that pathology alone cannot.”
Next, Dr. Whitworth provided a summary of clinical results. “I still hear in tumor boards that a young woman (age <50) with a high-grade DCIS obviously needs RT. This new data has demonstrated that grade and age do not accurately distinguish the patients who have a low-risk or who will benefit from RT. These clinpath features help, but they can’t really discriminate between those groups.”
“So, here is what we found in this comparison when you can discriminate between these groups biologically, using DCISionRT. We see no statistically significant difference in invasive risk for the age <50 and/or high-grade patient compared to the age >50 and grade 1 or 2, and almost no benefit to RT. Whereas, in the elevated and the RRt risk groups we see a high risk without RT and a substantial benefit to RT, regardless of age or grade.”
“The takeaway is ‘not all patients with DCIS need the same treatment’. The DCISionRT test provides the ability for individualized patient care via personalized risk and RT benefit assessment.”
To listen to the entire webinar, including case studies and questions, click here
Pat Whitworth, MD, FACS, Breast Surgical Oncology Specialist and Director of the Nashville Breast Center
Chirag Shah, MD, Co-Director of Comprehensive Breast Program and Director of Clinical Research in the Department of Radiation Oncology at the Cleveland Clinic
Troy Bremer, PhD, Founder and Chief Scientific Officer, PreludeDx